Author’s note: This current discussion is intended to be relatively detailed with more specific citation support, and refers to the other link for practical recommendations. A relatively short and practical guide is available at this link: Link to “Lightweight Aprons Exposed”
The regulations for testing and labeling of X-ray protective clothing are surprisingly lax (13, 30). We don’t know what we are getting without laborious in-house testing, especially with the newer non-lead or lightweight varieties (3, 6, 2, 4). Claims of light weight protective lead equivalent aprons are followed by disappointment as the true results become known. The strong energy-dependency of attenuation, which is very different for the non-leads relative to lead (3, 1, 2, 4, 15, 16, 5, 17) and the importance of testing non-leads with broad beam geometry to detect the secondary fluorescent radiation that they produce (1, 4, 15, 19, 16, 5, 18) means that many non-leads are reported at energies and geometries that allow their Pb equivalence to be overstated on the label (15). Non-lead materials are not providing the results that were expected of them unless they too are made into heavy aprons, and even then the protection can be erratic and counter to label. Interventionalists must exercise great caution as they balance comfort vs. protection
Busy interventionalists need good protective shielding, generally accepted to be at least equivalent to 0.5 mm Pb. Although imaging chain advances have caused reductions in dose/minute, operator doses are pushed up over recent years and decades by more specialized practices and continually increasing complexity of procedures. Radial access increased fluoroscopy times (20), and very intensive procedures such as TAVR and fenestrated EVAR are now common. Often overlooked is the huge impact of the worldwide obesity epidemic (21,22) since larger patients cause several-fold increases in operator exposure, described in one study to be 8.4X when increasing patient thickness from 24 to 34 cm (23). Lifetime operator doses are generally unknown since they are not tracked as interventionalists move between institutions and jobs, compliance with consistent badge-wearing is as low as 63% (24), and under-lead badges are frequently not used. It is incumbent on the interventionalist to make certain they are adequately protected with suitable protective clothing, yet the products are less protective than they were in the past as manufacturers sell large numbers of lightweight aprons, frequently without lead, which pass through the loose regulatory system without providing the protection that users believed they were receiving. They only way to insure adequate self-protection is to gain an understanding of the principles and take precautions as outlined in this discussion and elsewhere (Link to “Lightweight Aprons Exposed”). The only fast way to improve the problem at large, since regulations are very unlikely to change enough in the near future, is to become picky customers who force vendors to provide more information than required by law in order to earn their sales.
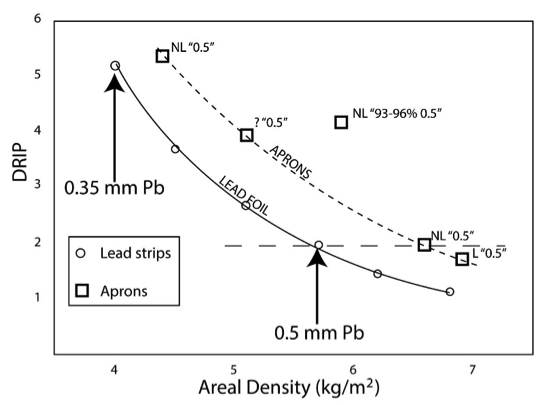
When tested independently by academic physicists using methods which are more accurate than those routinely performed by manufacturers and hospital physicists or RSO’s, lightweight aprons frequently underperformed relative to their labels (3, 6, 1, 7, 2, 4, 15, 17, 25) causing some authors to recommend internal validation (6, 7, 4, 17, 25, 26). In one report, 73% of 41 aprons were outside tolerance levels, with discordance between label and actual Pb equivalency in 3 of 4 manufacturers (6). Another study found the non-lead aprons to provide 70% lower attenuations compared to lead-based models, especially below 80kVp (1). This is especially concerning since these lower energies are particularly hazardous biologically (27). Another study confirmed higher than labeled transmissions for two non-leads ranging from 61% to 478% that of a lead apron, most markedly at the quality of 60 kVp (15). Studies have shown that protection depends on the weight of the garments, or more specifically the areal density (mass per area) (17, 25). Reducing weight through use of non-leads or using too little attenuating elements in the matrix of the apron causes attenuation to decrease, even when not reflected by the Pb equivalency rating on the label (a value which many think should be abolished in favor of reporting of transmission values) (17, 25). In one of the best studies on the subject, it was shown that lightweight non-lead garments were lighter because they provided lower protection, and not due to more efficient attenuation on a weight basis (17).
Since users are not being protected by regulations, and radiation safety officers often have their hands full trying to meet regulations without extra time to perform laborious tests, it becomes necessary for the user to understand some physics in order to make sure they are protected. There are two main principles playing roles; the different patterns of energy dependency of attenuation for the different metals, and the emission of fluorescent secondary radiation by different metals when exposed to certain energies found in scattered x-rays. This fluorescent radiation requires broad-beam geometry for detection in order to prevent overestimation of a material’s protective capability. It is also important to be aware that the labeled Pb equivalency of some aprons corresponds only to the overlapped zones without being declared.
Attenuating capabilities over the 30-150keV range of interest for the materials used in aprons is highly energy dependent (3, 1, 2, 4, 15, 16, 5, 18, 17). This is in large part due to the photoelectric effect, with the various metals having their own different k-absorption edges and emission lines (16). It is commonly known that the protection with lead-free aprons is strongly associated with beam quality, including the study showing the penetration through one lead-free garment at 60 kVp was 478% higher than the penetration for the lead-based garment of similarly labeled Pb equivalency (15). Whereas Pb and the non-Pb apron materials may be equivalent at one beam quality measured by manufacturer, they may be very greatly different at others to which the operator is constantly being exposed (3, 1, 2, 4, 15, 16, 5). These factors can cause great overestimation of the protective capability of many aprons, especially non-lead. As said nicely in one report: “…as lead has been replaced by other elements, verifying manufacturers’ claims regarding the lead equivalence of such garments has become nearly impossible, and current standards only require measurement of attenuation or lead equivalence at a single beam quality. A garment may provide a high degree of protection at the specified beam quality, but underperform at others.” (15).
These differences can be used to advantage in the mixtures of materials with lead (4) to reduce weight slightly without substantial loss of protection compared to pure lead, but lightweight non-lead preparations have led to the disappointing results described above.
When apron materials, particularly the non-leads of lower atomic number, are exposed to the scatter radiation field, they emit a new secondary radiation called fluorescence, which is typically of lower, biologically damaging energies that penetrate the shallow organs such as breast tissue, male gonads, thyroid, and skin (1, 4, 5, 15, 19, 16, 5, 18, 27, 28). This secondary radiation is most important for shields near the body, such as aprons (5). The relative biological effectiveness (RBE) of transmitted and secondary radiations can be doubled with some non-leads compared to lead materials (27). This difference was shown to be more pronounced at lower transmission values (28) when the user may be the least concerned. Narrow-beam geometry testing (Link to figure of narrow beam) is the most commonly used and simplest setup for testing apron materials, but does not detect this fluorescent radiation, and therefore overestimates the attenuation profiles of many non-lead aprons (1, 4, 15, 19, 16, 5, 18). Fluorescence is detected with broad-beam geometry Link to figure of broad beam which is less commonly available and not required for labeling (1, 4, 15, 19, 16, 5, 18). Any apron which is not predominantly lead based should be tested under broad beam geometry and explicitly stated on the label. A German study showed that three lead-free aprons which passed manufacturer criteria failed to fulfill the criteria when tested according to the recommended but optional German DIN 6857-1 standards, and that the only apron which passed was lead-based (2). Non-lead bilayers were designed to minimize the fluorescent effect, but one study of such a preparation showed 20-30% higher air kerma transmissions for surface radiation compared to penetrating radiation (16). Narrow beam testing was adequate in the past when aprons were all predominantly lead but should be eliminated in modern day since it is used inappropriately, albeit legally, with the user suffering the consequences.
The following example occurred in our department. A physician colleague purchased a lightweight skirt and vest to help with his back pain, after assurances from the salesman that it was rigorously tested to earn its labeled Pb equivalency of 0.5 mm front and 0.25 mm back. Intrigued by its lightness, we performed a crude test using an electronic dosimeter and compared the front of the vest to another heavier lead apron which was also labeled 0.5 mm Pb in front. Surprised by the difference, we passed the vest to our physicist for official testing and comparison to 2 other aprons, with the following results:
Figure 1. Transmission of x-rays at 80 kVp narrow beam geometry:
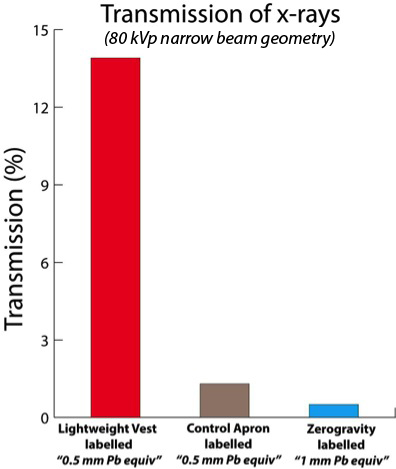
| “Lightweight” vest labeled (0.5 mm Pb equiv): | 13.9% |
| Control apron (labeled 0.5 mm Pb equiv): | 1.3% |
| Fabric from Zero-Gravity™ suspended system (labeled 1.0 mm Pb equiv): | 0.5% |
The lightweight vest allowed 10.7 X the radiation transmission compared to the control apron, yet both were labeled as having 0.5 mm Pb equivalency. This large difference is shocking to somebody who might have spent hundreds or thousands of hours in such an apron, thinking it was equivalent to another apron because both were “equivalent” to 0.5 mm Pb on their labels.
The discrepancy can be due to a combination of the factors described above, possible poor testing quality, and another common cause: some manufacturers label Pb equivalency based on overlap of front flaps. In other words, it may only apply to the segment where overlap occurs, without disclosure by label, website, or salesman. The thickness is therefore only ½ as much as the user expected. Since the preponderance of the vest and skirt are not overlapped during use, including the anterolateral portion where a large proportion of the scatter enters during most vascular procedures, exposure may be much higher than expected. We examined the vest under fluoroscopy, demonstrating that the back and front were the same attenuation despite being labeled as different, and both were much lower in attenuation than the other apron. The simple way to determine this is described in Link to “Lightweight Aprons Exposed”
But even when tested overlapped, the lightweight vest still under-performed by a factor of 3-fold transmission (3.9% vs 1.3%) compared to a non-overlapped standard apron labeled at the same lead equivalency, and may have fared even more poorly if tests using broad beam geometry at multiple energies were performed.
A single thickness of the material from a Zero-Gravity ™ suspended radiation protection unit (labeled 1.0 mm Pb equiv) was tested using the same equipment and method described above, showing a transmission of 0.5%. This attenuated 27.8X better than the lightweight vest where it is not overlapped, 7.8X the lightweight vest when doubled over, and 2.6X as well as the 0.5 mm Pb control apron. A large study examining many methods and shielding habits showed that the presence of 1 mm Pb protective garment was the single greatest determinant of total body exposure besides caseload, reducing under-garment exposures by 2/3 (9).
Another way to cut weight in an apron is to skimp on the binding matrix and structural components. This can lead to breakdown and diminished attenuation. A lightweight apron was used for many procedures over years in our department. Upon periodic integrity check, the attenuating materials had substantially shifted, leaving large patches of poor protection. This was much to the dismay of the apron’s user, who wondered how many hours of fluoroscopy were performed in this condition before discovery. Aprons have different methods of binding the attenuating materials which should be considered, and integrity checks performed regularly (10).
Many factors have set the stage for confusion and discrepancies between labels and true performance. Regulations and reporting requirements are very loose, completely counter to the expectations of interventionalists who are accustomed to the strict regulations surrounding patient-related products and policies. Testing and reporting standards are outdated, inadequate, optional, and way too confusing to be understood by users, in addition to being copyrighted and lawfully available only by individual purchase. Citations of such standards by the vendors gives users a false sense of confidence about the products which nevertheless vary greatly in protection despite identically labeled Pb equivalency values. Users may be desperate to believe in promises of “lightest aprons on the market” or amazing proprietary fabrics because they are having discomfort, pain or worries about disability, but in reality miracle products don’t exist and a few basic metal compounds are used. There is a large gap between perception: I am protected because the label says 0.5 m mPb, there are certificates posted all over the website, and regulatory bodies are making sure it’s all meaningful –and the reality: regulations are almost non-existent, and the certificates and label don’t change the fact that the lightweight apron protects far less than the heavier one.
Regulations: Radiation protective clothing is an FDA Class I device, the lowest possible (17). Regulators reserve the right to audit manufacturers’ claims, but manufacturers are essentially self-policing. While radiation safety officers (RSO) periodically surveille aprons, vests, and skirts for defects such as tears and holes, the shielding power, arguably the most important component of the apron, is usually taken from the manufacturer’s labels at face value. The RSO may test the apron’s attenuating power when asked, however, this is not performed routinely and most will not have the means to provide truly meaningful data for all types of aprons. The awareness of the problems with lightweight and non-lead aprons comes nearly entirely from independent academic study and reporting in peer-reviewed medical physics journals, not from regulatory oversight.
Standards: Standards are available for purchase under copyright so are not viewable to most users or even their RSO’s. Manufacturers buy them and have the option to choose which to use, if any. They may contract unregulated third parties to do the testing. So the certificates claimed by manufacturers are not from centralized regulatory bodies or the standards bodies. The standards arose with lead-based aprons and work reasonably well for them, but not for non-lead models as explained in detail below. They provide many options for how to test and report, and some options are not considered appropriate for non-lead lightweight aprons by several authors. The testing is of small patches of material and not on actual aprons, so considerations due to configuration, such as overlap, are not accounted for, causing misleading results as explained below. It is possible for a material to be tested according to a standard such as ASTM (8) with regard to attenuation values which the user may not be able to find or understand, while the label is reported in Pb equivalency, which can grossly overestimate protection and, according to ASTM is not provided for in their standards and not recommended as noted in their statement: “Although lead equivalency has been the standard for reporting protective material capability, the drafters of this test method believe it is not feasible to obtain adequate standard lead samples for reporting lead equivalency values.”(8) Other criticisms of ASTM (designation F 2547-06): energy range is not broad enough (should include lower and higher kVp’s), uses direct beam whereas operators are exposed to scatter of a different quality, uses excessive beam hardening, permits use of narrow-beam geometry which can grossly underestimate exposure (see below), provides vague description of test setup. DIN standards are written in German. IEC standards (29) have recently been improved to some degree (IEC-616331-1: 2014-05 and IEC-616331-3:2014-05 [must have “2014” in title]). IEC-616331-1: 2014-05 is sometimes cited without IEC-616331-3:2014-05, leaving out much of the requirements specific to aprons and other garments, and permitting narrow beam geometry and as few as 2 radiation qualities defining a range, selected from a broader table. IEC-616331-3:2014-05 should be cited also, but is only properly done in compliance with the document when the report includes name of manufacturer or supplier, designation of type of apron, lead equivalent, x-ray tube voltage range which should be 50-110kV, area density of fabric in the garment, and “IEC 61331-3:2014” exactly as stated here. Absence of any of this information, marked clearly and permanently on the garment, indicates non-compliance with this standard. Also required on accompanying documents (not on the garment itself) is specific information about the size of and length and portions of body covered. This author has not seen such labels on garments at trade meetings in the U.S. Because compliance is optional and confusion exists, we recommend the buyer request written attestation for non-lead garments that the lead equivalents were tested with inverse broad beam geometry or broad beam geometry, with specific lead equivalents at each beam quality of 50, 70, 90, and 110 kv. And that anything labeled “front” covers 60% of the circumference of the body of a user who fits the garment (approximately from left to right posterior axillary lines). Although a step in the right direction, the problems are far from solved and the effects of these optional standards on actual product quality will take years before independent academic studies can determine if they have had any substantial effect.
Even if the standards were stricter, they still wouldn’t prevent a common cause of misunderstanding. Manufacturers make claims such as “certified to the exacting standards of [IEC or AST or DIN], leading to the misperception that these organizations require certain results to be achieved to grant a “certification.” In reality, the standards do not certify anything, they are simply guidelines for testers on how to test and report results. Moreover, the standards do not require any certain results to be achieved; they do not describe a bar over which the product must clear. The results could be terrible, with very poor attenuation, yet still be in accordance with the “exacting” standards described. A piece of cardboard could be tested by nearly anybody in his own lab, who then provided a “certificate” indicating that he followed the guidelines of IEC or ASTM or DIN. The manufacturer might then claim that the piece of cardboard was “certified to the exacting [e.g. IEC] standards…” though its attenuation was essentially 0. For a real apron product, any existing certificate is probably created and signed by a member of the company or somebody they hired to test for them. These certificates are not required to become public and are often very difficult or impossible to extract from the manufacturers. Once obtained, it is still often difficult to tell if the apron you are considering is made from the material described in the certificate, or whether the thickness of material tested corresponds to the exact thickness of the apron, since most are constructed of a number of layers of the material, and that number is not disclosed with regard to the apron. Upon inquiry, the vendor’s representatives often don’t know the answer, and more inquiries to actual shop people are needed for informal and verbal results provided by the more helpful manufacturers. Also, the certificates are not for the aprons themselves, they are just for the material fragments tested, so whatever process of configuration or manufacture which might affect protection is not reflected.
In summary, determination of protective capability of an apron from vendor supplied information requires the diligence and shrewdness of a detective in order to succeed in only some of the cases (26). Self-testing, although laborious, seems to be the only way if one wants to venture towards lighter products or non-lead aprons. Hopefully someday each apron will have a permanently attached label giving all the information necessary to determine its protection, the information will be reliable, and there will be substantial repercussions to manufacturers or testers providing inaccurate or inconsistent information.
Many authors have called for changes in the testing and reporting standards (15, 6, 1, 2, 4, 5, 12, 17). The concept of Pb equivalency is no longer useful with the non-leads being used today with all the problems of comparing to lead described above, in addition to the difficulties in finding lead samples for comparison (17). The use of attenuation values is better, but would need to be available for all products to allow comparisons, and does not clearly give the user a good understanding of the apron without comparisons or charts of values for accepted standards. The best method would be to report transmission values at the various beam qualities (kVp’s and spectral descriptions), supplied with comparisons to lead for easy reference, since the transmitted radiation is what exposes the user (17, 25). This allows the user to easily see how much radiation they would receive with one product vs. another, or vs. a Pb equivalency standard. For example, a difference in attenuation from 99% to 94% may not sound like much, but it would mean that the user would receive 6X as much transmitted radiation for one vs the other. Other changes would include the requirement, not the option, to report at 30 kVp, 150 kVp, and three intermediate values which are consistent for all products, using standardized beam filtration qualities. Broad beam or inverse beam geometry should be mandatory. Values should not apply to double thickness in the overlap zones unless the overlap zones are complete from neck to bottom and from the poster axillary line on one side to the other for the largest person who might wear that size of apron. It should be mandatory to report the test values and the manner of labeling overlap on the label with enough information so that the user can be assured all of the above procedures were followed. IEC-616331-1: 2014-05 and IEC-616331-3:2014-05 have taken steps in these directions but not far enough, and leaving too many choices to the testers so that not all must be followed and comparisons for aprons tested in different ways are still difficult. Also the standards must be mandatory to be effective. Consideration of methods which emulate the actual scatter beam qualities of the real environment would be an excellent final step (15, 17).
With all the challenges still in place, choosing an apron is still very difficult. Guidelines are available at Link to “Lightweight Aprons Exposed”. In short, the simplest way to be reasonably assured of adequate protection is to buy an apron which is predominantly lead, with Pb equivalency rating of 0.5 mm, and to make certain that rating does not apply only to the overlapped portion, which may require careful fluoroscopy and comparison to an available standard as described in Link to “Lightweight Aprons Exposed”. If it feels good, test it; a light apron is a tip-off that something is wrong, since the lighter ones test unfavorably when tested carefully as in the references cited. If an apron feels heavy, it will usually provide the protection as labeled, although for some non-leads there is still some risk that its protection may be lower than expected, corresponding to the outliers that have been encountered in some studies (17, 25).
The message of ALARA (As Low As Reasonably Achievable) for the interventionalists is not to use regulatory limits to set our dose goals because we should strive to be well below them. Individual interventionalists are encouraged to work towards a safer environment for themselves and advocate for improved protection.
APPENDIX A:
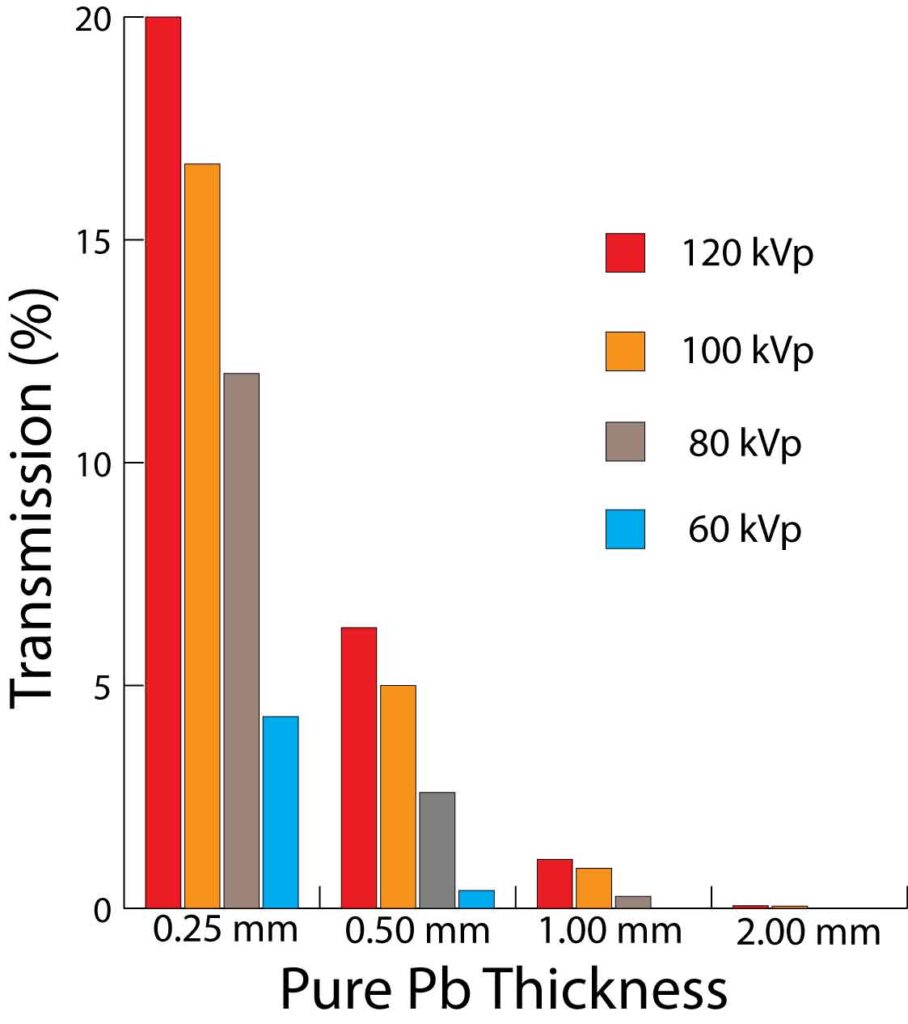
Appendix Table A. Effective transmission (%) with pure lead (Pb) by radiation quality. From (12) unless otherwise indicated in superscript:
| kVp | 0.25 mm Pb | 0.50 mm Pb | 1.0 mm Pb | 2.0 mm Pb |
| 60 | 4.3% | 0.4 | 0.01 | 0 |
| 70 | 5.44 | 0.94 | ||
| 80 | 12 | 2.6 | 0.27 | 0.01 |
| 100 | 15416.7 | 545 | 0.9 | 0.05 |
| 120 | 20 | 6.3 | 1.1 | 0.06 |
Appendix Figure A. Table A in graph form.
REFERENCES:
7. Vaiciunaite N, Laurikaitis M, Laurikaitiene J, Cerapaite-Trusinkiene R, Adlys G. Verification of lead equivalent for protective aprons used in radiology. Ninth International Conference & Workshop “Medical Physics in the Baltic States” 2011. Available from: http://www.medphys.lt/medphys2011/images/contributions/MedPhys2011_01_03_Vaiciunaite.pdf.
8. ASTM International. Standard test method for determining the attenuation properties in a primary X-ray beam of materials used to protect against radiation generated during the use of X-ray equipment. Designation F2547-06. Available through www.astm.org.
12. McCaffrey JP, Shen H , Downton B, Mainegra-Hing E. Radiation attenuation by lead and nonlead materials used in radiation shielding garments. Medical Physics, 2007 Feb; 34 (2):530-
13. US Food and Drug Administration [Internet]. Silver Springs (MD) [updated 2014 Sept 1; cited 2014 Sept 24]. Available from: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=892.6500.
14. INFAB Corp [Internet]. [cited 2014 Sept 24]. A challenge to BLOX-R and a warning to anyone involved in the use or procurement of flexible radiation materials. Available from: http://www.infabcorp.com/open-letter-to-bloxr/.
15. Jones AK, Wagner LK. On the futility of measuring the lead equivalence of protective garments. Med Phys 2013 Jun;40(6):063902-2:063902-9. doi: 10.1118/1.4805098.
16. McCaffrey JP, Mainegra-Hing E, Shen S. Optimizing non-PB radiation shielding materials using bilayers. Med Phys 2009 Dec;36(12):5586-5594.
17. Pasciak AS, Jones AK, Wagner LK. Application of the diagnostic radiological index of protection to protective garments. Med Phys Vol 42 (2) Feb 2015: 653-662.
18. McCaffrey JP, Tessier F, Shen H. Radiation shielding materials and radiation scatter effects for interventional radiology (IR) physicians. Med Phys 2012 Jul;39(7):4537-4546. doi: 10.1118/1.4730504. nts. Med Phys 42(2) Feb 2015: 653-662.
19. Pichler T, Schopf T, Ennemoser O. Radiation protection clothing in X-ray diagnostics – comparison of attenuation equivalents in narrow beam and inverse broad-beam geometry. Rofo 2011 May;183(5):470-476. doi: 10.1055/s-0029-1245996.
20. Feldman DN, Swaminathan RV, Kaltenbach LA, Baklanov DV, Kim LK, Wong SC, Minutello RM, Messenger JC, Moussa I, Garratt KN, Piana RN, Hillegass WB, Cohen MG, Gilchrist IC, Rao SV. Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention: An updated report from the national cardiovascular data registry (2007–2012). Circulation 2013;127:2295–2306.
21. Centers for Disease Control and Prevention [Internet]. Atlanta (GA) [updated 2014 Sept 9; cited 2014 Sep 24]. Available from: http://www.cdc.gov/obesity/data/adult.html.
22. World Health Organization [Internet]. c2014 [updated 2014 Aug; cited 2014 Sept 24]. Obesity and overweight. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/.
23. Schueler BA, Vrieze TJ, Bjarnason H, Stanson AW. An investigation of operator exposure in interventional radiology. RadioGraphics 2006;26:1533-1541. doi: 10.1148/rg.265055127.
24. Klein, LW, Tra Y, Garratt KN, et al. Occupational health hazards of interventional cardiologists in the current decade. Catheterization and Cardiovascular Interventions 2015. 86 (5) 913-924, November 1.
25. Lichliter A, Gipson S, Heithaus E, Syed A, Weir V, West J. Clinical evaluation of protective garments with respect to garment characteristics and manufacturer label information. Presentation and poster at the International Symposium on Endovascular Therapy (ISET) 2016, February 6-10, Hollywood Florida. Abstract: J Vasc Interv Radiol 2016;27:e1-e21, page e1-e2. http://www.jvir.org/article/S1051-0443%2816%2900020-8/pdf Abstract and Poster: https://www.eventscribe.com/2016/posters/ISETCIO/SplitViewer.asp?PID=MjYyNjA1MDAyNQ
26. Heithaus RE, Onofrio A, Weir V, Rees CR. Can aprons be properly evaluated for their protective quality without in-house validation? Poster at the International Symposium on Endovascular Therapy (ISET) 2016, February 6-10, Hollywood Florida. Abstract: J Vasc Interv Radiol 2016;27:e1-e21, page e11. http://www.jvir.org/article/S1051-0443%2816%2900020-8/pdf Abstract and Poster: https://www.eventscribe.com/2016/posters/ISETCIO/SplitViewer.asp?PID=MjYyNjg3MDAwOQ
27. Schmid E, Panzer W, Schlattl H, Eder H. Emission of fluorescent x-radiation from non-lead based shielding materials of protective clothing: a radiobiological problem? J Radiol Prot 2012 Sept;32(3):129-139. doi: 10.1088/0952-4746/32/3/N129.
28. Akber SF, Das IJ, Kehwar TS. Broad beam attenuation measurements in lead in kilovoltage X-ray beams. Med Phys 2008;18:197–202. doi: 10.1016/j.zemedi.2008.04.008.
29. International Electrotechnical Commission [Internet]. c2014. [cited 2014 Sept 24]. Available from: http://webstore.iec.ch/Webstore/webstore.nsf/ArtNum_PK/49622!opendocument&preview=1
30. http://www.infabcorp.com/is-your-lead-apron-protecting-you/ Access date 2-23-2016
APPENDIX B (Interesting excerpts from other publications):
“Therefore, under the experimental conditions described above, for an average weight reduction of 28% the lead free aprons allow on the average a 73% increase in transmission at 70 kVp and a 31% increase in transmission at 100 kVp when compared with the lead-containing 0.5 mm lead equivalent aprons.” (4)
“The manufacturers should be required to standardize their methods of transmission measurement and devise methods to minimize batch-to-batch variability…manufacturers should also be required to present transmission curves at a range of kVp values in their product literature. Enforcement of the lead equivalent requirement or specification might fall under the auspices of the FDA or some other federal government agency.” (4)
“Of note, 18.5% of the respondents self-reported occasional failure to wear personal radiation badges, and an additional 28.6% reported never wearing radiation badges. This practice was most prevalent in those aged 51–60 years, in whom 41.4% reported not wearing radiation badges at times and 39.5% routinely failed to wear badges (Fig. 1).” (24)
“In 2006, Americans were exposed to more than seven times as much medical ionizing radiation as was the case in the early 1980s, and the amount due to interventional fluoroscopy increased 33 fold.” (National Council on Radiation Protection & Measurements (Bethesda. MD). Ionizing radiation exposure of the population of the United States. Report No.:160. Available from: http://www.ncrponline.org/PDFs/2012/DAS_DDM2_Athens_4-2012.pdf ) (Smith-Bindman R, Miglioretti DL, Johnson E, Lee C, Feigelson HS, Flynn M, Greenlee RT, Kruger RL, Hornbrook MC, Roblin D, Solberg LI, Vanneman N, Weinmann S, Williams AE. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA 2012 Jun 13. Available from: http://jama.jamanetwork.com/article.aspx?articleid=1182858&resultClick=3 )
“Almost every manufacturer makes the claim that their aprons are “the lightest on the market”. While there are miniscule differences in the weights of the powders used to produce radiation protection materials, the simple truth of the matter is, there are no secret formulas and almost all apron manufacturers use variations of the same metals in their products. The bottom line here is, if it’s lighter weight, it is not offering the same protection levels. Plus or minus a very small percentage, a true .50mm LE apron is going to weigh the same from one manufacturer to the next.” (30) Access date 2-23-2016