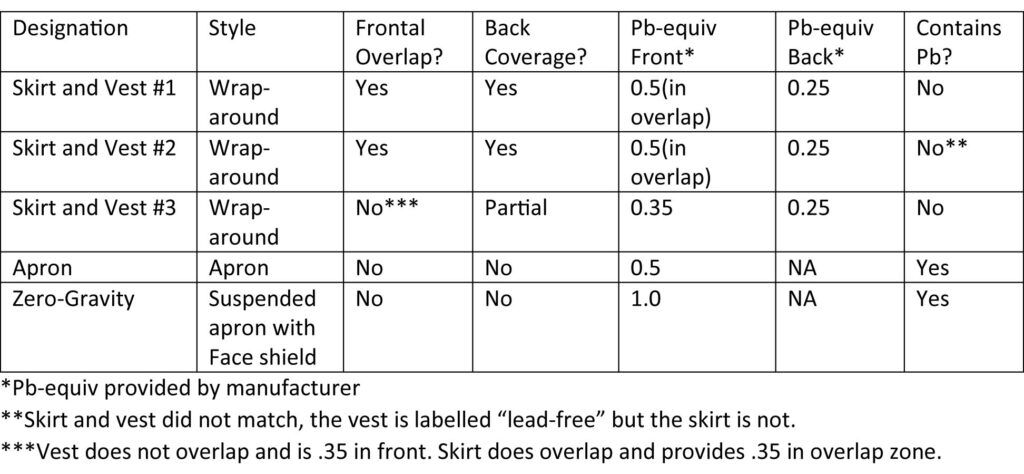
ABSTRACT: Many different personal radiation protection options are available today for use by interventionalists in their suites. This study examines a variety of options to determine the importance of lead vs. lead-free, back coverage vs. none, and frontal overlap vs. none. Secondary scatter was provided by a stack of acrylic (phantom patient) and exposure was measured for the phantom operator (a life-size frame “wearing” the personal protection) while standing in a typical position during fluoroscopy. The results show that operator exposure is mostly influenced by the attenuation properties of the protective material and that garments with open backs often protect better than wrap around styles due to lesser attenuation capacities of the material used in the latter, and because secondary scatter from other objects in the room is far lower than the frontal primary scatter from the patient even after penetration of the material. The results also raise concerns as cited in other reports about the attenuating power of styles which employ: 1. Labeled Pb-equivalency only in the overlap zones, leaving the sides with lower attenuation, 2. Lead-free varieties whose Pb-equivalency labels may not apply to the entire spectrum of scattered radiation in a clinical environment.
INTRODUCTION: This test of several personal protection garments and devices being used in an operational interventional suite was performed to examine the variability of their attenuations of the scattered radiation, as well as the impact, if any, of whether or not they cover the operator’s back.
METHODS: Protective devices tested (all currently in common use):
Date of test: 18.07.2015 X-ray equipment: Philips Allura Clarity. Functional clinical suite Dosimeter: Victoreen 451P. Calibration date: May, 2015
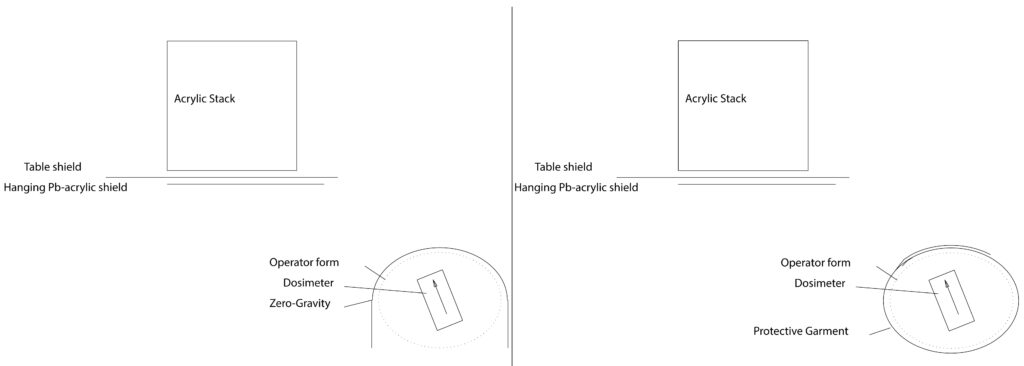
Test Phantom patient: Stack of acrylic slabs 38 cm X 38 cm X 24 cm height
Operator Form: Life-size torso model made of a lightweight wooden frame (mostly open space) supported by a support pole (hollow aluminum tube). This serves as a support for the protective garments, which are held in a similar shape, configuration, and location as if worn by a real operator. It also supports the dosimeter which is positioned inside the garment at the level of the abdomen.
Position of Phantom Operator: Positioned at a typical location for an abdominal interventional procedure (see schematic Figs). The dosimeter is located 82 cm from the center of the phantom patient (59 cm along x axis and 57 cm along y axis). The dosimeter height is 112 cm from floor. Measurements were obtained with the dosimeter rotated into several orientations around the clock-face (at 12:00, 1:30, 3:00, 4:30, 6:00, 7:30, 9:00, and 10:30), and the highest value was used. The operator phantom was kept in same location for all different tests with different garments.
Background radiation measurement: <1uSv/h Settings
(dimensions in cm):
SID: 104
FD: 48
Height: 1 (display). 100 cm as measured to floor)
Fluoroscopy: “Fluoro-flavor 1” low dose.
Other shields: 0.5 mm Pb-equiv acrylic hanging shield in typical working position, and with standard table-mounted shielding strips in place.
RESULTS:
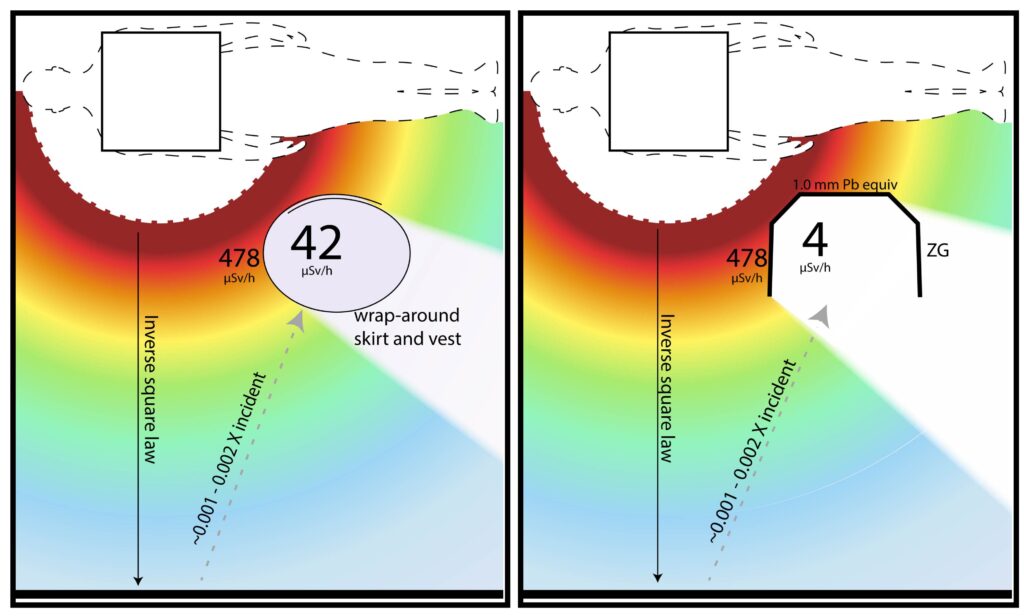
Kv=80, mA=18.
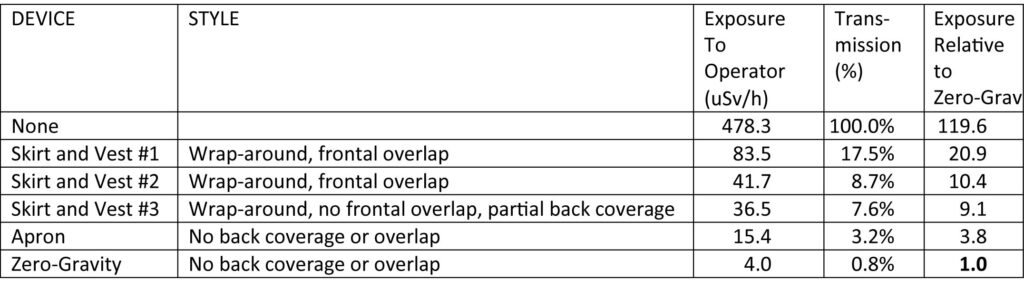
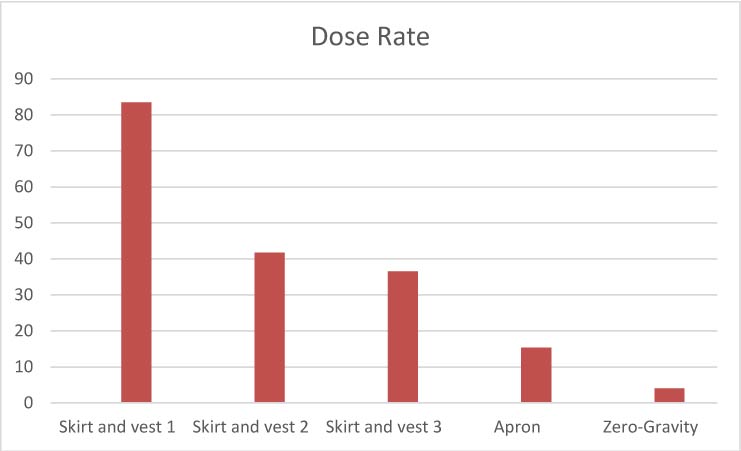
CONCLUSIONS: Exposures to operator are highly variable for the different garments. The two highest exposures were for the wrap-around skirt and vest garments with the most complete back coverage. Skirt and vest #3 had incomplete back coverage but provided lower operator exposures than the first two, due to its better attenuation properties. The apron and Zero-gravity ™ have front and side coverage only, but both showed lower exposures than the wrap-around garments presumably due to their higher Pb equivalencies and attenuating properties. This reduction of exposure was most notable for Zero-gravity ™ which may utilize the highest Pb equivalency since it is not supported by the operator. These findings are consistent with the widely accepted concept that exposure to the operator’s back due to secondary scatter from the floors, walls, and other objects in the room is negligible compared to the much larger primary scatter from the patient and table within the beam, which is directed at the front and sides of the operator, and whose attenuation will depend largely on the degree of attenuation by the garment material (1). The radiation passing through the front and sides of the garments is more than the amount which could be scattering to the back from the walls and floors. The decreases in exposure to the head and lower legs where shielding is provided by Zero-Gravity ™, but not by the other garments, was not assessed in this test. The predominant significance of the attenuating capacity of the garment material was also noted in a long-term multi-center clinical study with real patients and operators. Of the multiple factors examined, the two most significant were Pb-equivalency of the garment and case-load (2).
- Brateman L. The AAPM/RSNA Physics Tutorial for Residents. Radiation safety considerations for diagnostic radiology personnel. Radiographics 1999;19:1037-1055. http://pubs.rsna.org/doi/full/10.1148/radiographics.19.4.g99jl231037
- Marx MV, Niklason L, Mauger EA. Occupational radiation exposure to interventional radiologists: A prospective study. J Vasc Intervent Radiol 1992;3:597-606.
FURTHER DISCUSSION:
The results of this study are not surprising in view of previous studies as well as the accepted values for attenuation by varying thicknesses of Pb. Transmission (1-attenuation) of Pb for energies in the spectrum of scattered fluoroscopic x-rays is shown below (data from McCaffree et al [2]).
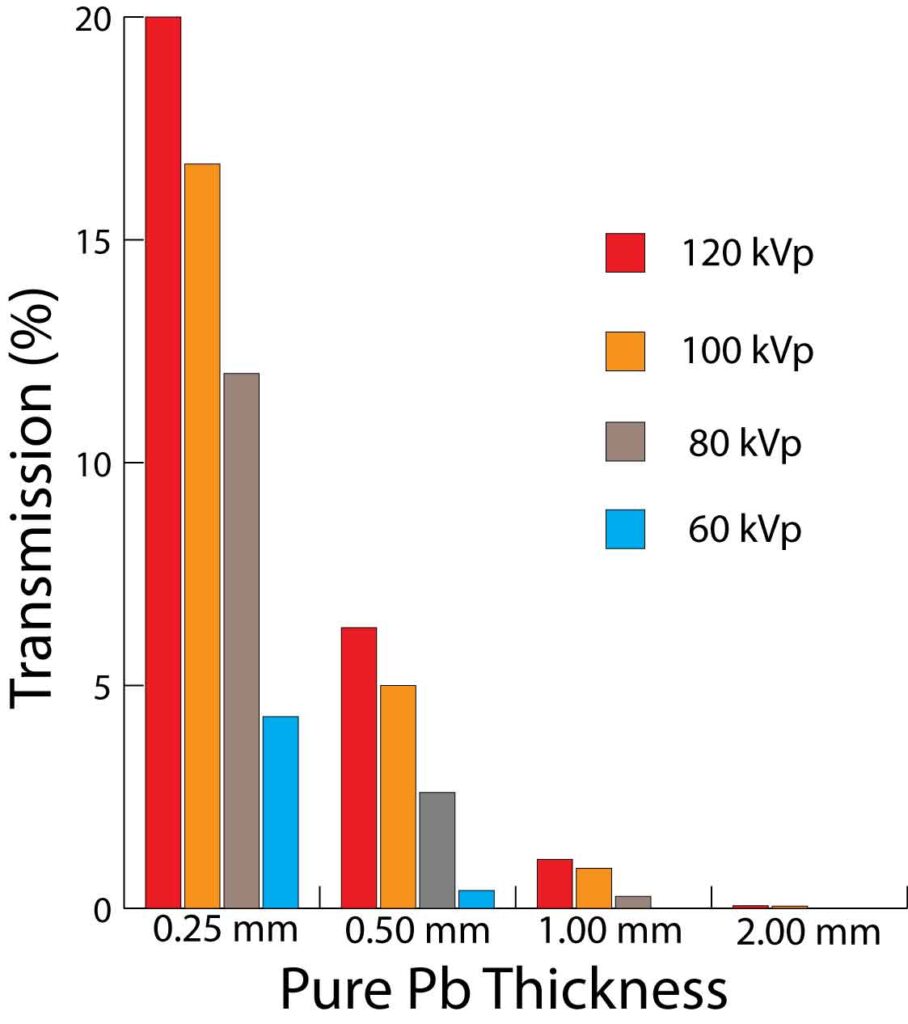
The reported transmissions for 0.5 mm Pb vs. 1.0 Pb in the graph correlate rather well with the 3.85 fold difference in operator dose-rate between Zero-Gravity ™ and the 0.5 mm Pb lead apron. The 2.4 fold difference between the 0.5 mm Pb lead apron and the 0.35 mm Pb equiv skirt and vest #3 does not seem far out of line with what one might estimate when looking at the above transmission graph although the comparison is somewhat more difficult due to the pure Pb thickness tested. However, the markedly reduced attenuations provided by skirt and vest #1 seems out of line with expected. Possible causes include:
- Reduced attenuation of the non-lead material below what would be achieved by Pb across the spectrum of scattered energies, and
- The dependence on frontal overlap for full labeled Pb equivalency which allows higher transmissions at the sides and anterolateral area where much of the scatter is directed at the operator in typical working positions.
Although this study is too small to determine the relative contributions of these two factors, it is likely that both are involved. Many previous reports have already shown that the labeled Pb equivalency of non-lead aprons often poorly reflects actual attenuations of scattered radiation, overestimating them substantially in some cases (3-10). Several authors have recommended that this labeling system be replaced by a more useful and accurate report of the attenuations at several energies across the range seen in scattered diagnostic x-rays (60-120 kv) (4,5,7,8,9-14). This current study supports previous works concluding that the user may not know what to expect from non-lead fabrics with the current labeling system without doing laborious testing of their own as we have done. We strongly encourage all users working near the patient who are considering lightweight garments to test them at several energies regardless of label information. We have not found a highly protective garment which felt light.
REFERENCES:
1. McCaffrey JP, Shen H , Downton B, Mainegra-Hing E. Radiation attenuation by lead and nonlead materials used in radiation shielding garments. Medical Physics, 2007 Feb; 34 (2):530-7.
2. Muir S, McLeod R, Dove R. Light-weight lead aprons—light on weight, protection, or labeling accuracy? Australas Phys Eng Sci Med 2005 Jun;28(2):128-30.
3. Finnerty M, Brennan PC. Protective aprons in imaging departments: manufacturer stated lead equivalence values require validation. Eur Radiol 2005 Jul;15(7):1477-84.
4. Eder H, Panzer W, Schofer H. Is the lead-equivalent suited for rating protection properties of lead-free radiation protective clothing? Rofo 2005 Mar;177(3):399-404.
5. Vaiciunaite N, Laurikaitis M, Laurikaitiene J, Cerapaite-Trusinkiene R, Adlys G. Verification of lead equivalent for protective aprons used in radiology. Ninth International Conference & Workshop “Medical Physics in the Baltic States” 2011. Available from: http://www.medphys.lt/medphys2011/images/contributions/MedPhys2011_01_03_Vaiciunaite.pdf.
6. Eder H, Schlatt H, Hoeschen C. X-ray protective clothing: does DIN 6857-1 allow an objective comparison between lead-free and lead-composite materials? Rofo 2010 May;182(5):422-8. doi: 10.1055/s-0028-1110000.
7. Christodoulou EG, Goodsitt MM, Larson SC, Darner KL, Satti J, Chan HP. Evaluation of the transmitted exposure through lead equivalent aprons used in a radiology department, including the contribution from backscatter. Med Phys 2003 Jun;30(6):1033-8.
8. Jones AK, Wagner LK. On the futility of measuring the lead equivalence of protective garments. Med Phys 2013 Jun;40(6):063902-2:063902-9. doi: 10.1118/1.4805098.
9. Pichler T, Schopf T, Ennemoser O. Radiation protection clothing in X-ray diagnostics – comparison of attenuation equivalents in narrow beam and inverse broad-beam geometry. Rofo 2011 May;183(5):470-476. doi: 10.1055/s-0029-1245996.
10. Schlattl H, Zankl M, Eder H, Hoeschen C. Shielding properties of lead-free protective clothing and their impact on radiation doses. Med Phys 2007 Nov;34(11):4270-80.
11. McCaffrey JP, Shen H, Downton B, Mainegra-Hing E. Radiation attenuation by lead and nonlead materials used in radiation shielding garments. Med Phys 2007 Feb;34(2):530-537. doi: 10.1118/1.2426404.
12. ASTM International (West Conshohocken, PA). Standard test method for determining the attenuation properties in a primary X-ray beam of materials used to protect against radiation generated during the use of X-ray equipment. Designation F2547-06. Available through http://www.astm.org/Standards/F2547.htm.
13. International Electrotechnical Commission [Internet]. c2014. [cited 2014 Sept 24]. Available from: http://webstore.iec.ch/Webstore/webstore.nsf/ArtNum_PK/49622!opendocument&preview=1.
14. Brateman L. Radiation safety considerations for diagnostic radiology personnel. From: The AAPM/RSNA Physics Tutorial for Residents. Radiographics 1999;19:1037-1055.